Introduction: Delineating the Cognitive Landscapes of OCD and Pure O OCD
Obsessive-Compulsive Disorder (OCD) is a complex mental health condition characterized by unwanted and intrusive thoughts (obsessions) and repetitive behaviors or mental acts (compulsions) that a person feels driven to perform. Traditionally, OCD is recognized by its visible compulsions, such as excessive hand-washing, checking, or arranging objects in a particular way. However, a less visible but equally distressing form of this disorder is Pure O OCD, or Pure Obsessional OCD, where the struggle largely happens within the mind, often unnoticed by others.
The distinction between OCD and Pure O OCD lies not only in the visibility of symptoms but also in the underlying cognitive themes that drive these conditions. While OCD encompasses a broad range of obsessions and compulsions, Pure O OCD predominantly involves intrusive thoughts and mental rituals, often without observable compulsions. These internal battles can be as debilitating as the more visible symptoms of traditional OCD.
Understanding these conditions requires delving into the cognitive themes that characterize them. Pure O OCD is often defined by intense, intrusive thoughts and a relentless quest for certainty, manifesting in mental rituals and persistent self-doubt. On the other hand, traditional OCD includes themes such as contamination fears, the need for things to feel “just right,” and visible compulsions like checking or cleaning.
This article aims to explore and compare the cognitive themes inherent in Pure O OCD and traditional OCD. By examining these themes, we can gain a deeper understanding of how these disorders affect the lives of those who struggle with them. Additionally, this understanding is crucial for developing targeted and effective treatment approaches. Real-life examples will be used to illustrate these themes, providing a clearer picture of how they manifest in everyday situations.

Part 1: Understanding Pure O OCD
Definition and Explanation of Pure O OCD
Pure O OCD, or Pure Obsessional OCD, is a subtype of OCD characterized primarily by intrusive thoughts, urges, or images, with few or no observable compulsions. Unlike traditional OCD, where compulsions are often physical or visible, the compulsions in Pure O OCD are predominantly mental.
Key Cognitive Themes in Pure O OCD
- Intrusive Thoughts: Individuals with Pure O OCD experience persistent, unwanted thoughts or images that are often distressing and at odds with their values or self-image. These thoughts can include fears of harming others, unwanted sexual or violent images, or fears of saying inappropriate things.
- Urges without Compulsions: Pure O OCD is marked by intense urges or feelings that something is not right, yet the individual may not engage in visible compulsive behaviors to alleviate these urges, leading to significant internal distress.
- Fear of Acting on Thoughts: A common theme is the fear that one might act on intrusive thoughts, despite these thoughts being unwanted and not aligned with the individual’s true intentions.
- Overestimation of Threat: Individuals often overestimate the danger or significance of their thoughts, believing that having a thought is akin to the likelihood of it becoming real.
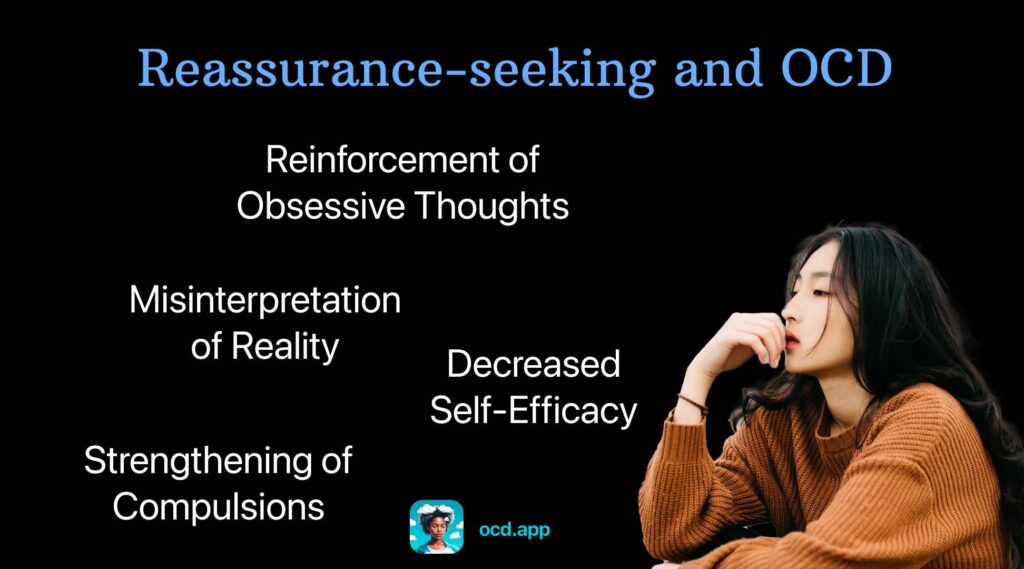
- Need for Certainty: There is a relentless quest for absolute certainty over thoughts and actions. This need can manifest in constant reassurance-seeking or mental review of events.
- Intolerance of Uncertainty: This involves difficulty in coping with the uncertainty and ambiguity of life’s events, leading to increased anxiety and distress.
- Fear of Losing Control: A pervasive fear that one might lose control and act on unwanted impulses or thoughts.
- Hyper-responsibility: Feeling an exaggerated sense of responsibility for preventing harm or ensuring no harm comes from their thoughts or actions.
- Avoidance Behaviors: Engaging in avoidance of certain situations, people, or activities that might trigger intrusive thoughts or increase anxiety.
- Mental Rituals: Performing internal rituals, such as counting, praying, or repeating phrases in one’s mind to neutralize or suppress intrusive thoughts.
- Self-Doubt: Persistent doubt about one’s own thoughts, feelings, and actions, leading to a constant internal struggle for clarity.
- Excessive Analysis: Tendency to overthink and overanalyze one’s own thoughts and behaviors, often leading to a cycle of rumination and increased anxiety.
In the next section, we will explore the cognitive themes prevalent in traditional OCD and how they compare and contrast with those in Pure O OCD.
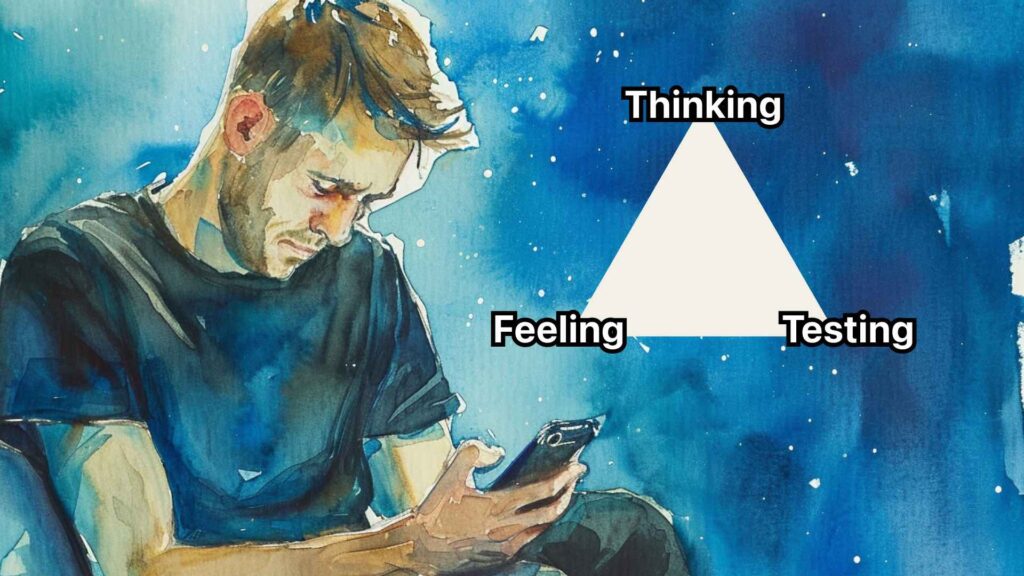
Quick Insight: What are compulsions?
Compulsions are like mental or physical rituals people with OCD feel they must do to ease their anxiety. Think of them as actions like washing hands a lot, checking things repeatedly, or even counting silently. They’re meant to prevent bad things from happening, but they don’t really stop these things and can take up a lot of time.
In short, compulsions are those repetitive things someone does to try and make their worry or stress go away, even if just for a little while.
Part 2: Exploring Traditional OCD
Definition and Characteristics of Traditional OCD
Traditional Obsessive-Compulsive Disorder (OCD) is a mental health condition marked by a pattern of unwanted thoughts (obsessions) and repetitive behaviors (compulsions) that are performed to relieve anxiety caused by these thoughts. Unlike Pure O OCD, traditional OCD usually includes more visible and tangible compulsive actions.
Key Cognitive Themes in Traditional OCD
- Contamination Fears: This theme involves intense fear of germs, dirt, or getting contaminated. It often leads to compulsions like excessive hand-washing, cleaning, or avoiding touching certain objects.
- Fear of Harm: Concerns about causing harm to oneself or others, either accidentally or deliberately. This can lead to compulsive checking of locks, appliances, and repeatedly seeking reassurance.
- Not Just Right Experiences: A feeling that certain actions or situations are not just right or perfect, leading to repetitive behaviors until the feeling is alleviated.
- Checking and Reassurances: This involves repeatedly checking things (like whether a door is locked) or seeking reassurance from others to alleviate fears or doubts.
- Fear of Self: Worry about one’s potential to cause harm or make significant mistakes, leading to avoidance or checking behaviors.
- Attachment Anxiety and Avoidance: Concerns about relationships and social interactions, often leading to compulsive behaviors aimed at ensuring the stability and security of these relationships.
- Importance of Thoughts: Overemphasis on the significance of one’s thoughts, such as believing that having a bad thought is morally equivalent to carrying out a bad action.
These cognitive themes in traditional OCD often lead to a cycle of obsessions and compulsions, where the individual feels compelled to perform certain actions to reduce the anxiety or distress caused by their obsessions. Unlike Pure O OCD, where the struggle is predominantly internal, traditional OCD usually involves more observable behaviors.
Quick Insight: What are Obsessions?
Obsessions are like persistent, unwanted guests in your mind. They are thoughts, images, or urges that pop up again and again, causing a lot of worry or discomfort. People with OCD often find these obsessions intrusive and hard to shake off. Imagine constantly worrying about germs, having doubts about safety, or experiencing distressing thoughts that just won’t go away. These obsessions aren’t just everyday worries; they’re more intense and can make someone feel really anxious or uneasy.
In short, obsessions are those nagging thoughts that stick in your head and keep bothering you.
In the next section, we will present real-life scenarios to illustrate each theme in both Pure O OCD and traditional OCD, and compare how these themes manifest differently in each condition.
Part 3: Real-Life Examples and Comparisons
In this section, we’ll explore real-life scenarios that illustrate the cognitive themes in Pure O OCD and traditional OCD, highlighting how these themes manifest differently in each condition.
Pure O OCD Examples
- Intrusive Thoughts: Jane constantly has intrusive thoughts about harming her loved ones, despite loving them deeply. She is tormented by these thoughts but does not act on them.
- Urges without Compulsions: Tom feels an urge to confess every minor mistake he thinks he has made at work, fearing catastrophic consequences. However, he doesn’t engage in any visible compulsive behaviors.
- Fear of Acting on Thoughts: Sarah is plagued with thoughts of shouting insults in a quiet room. She avoids social gatherings, fearing she might lose control and act on these thoughts.
- Overestimation of Threat: Kevin believes that if he thinks about a loved one getting into an accident, it will happen. This thought causes him extreme anxiety, although there is no rational basis for this belief.
- Need for Certainty: Emily spends hours analyzing past conversations, worried she might have said something offensive without realizing it.
- Intolerance of Uncertainty: Alex avoids making decisions, big or small, due to the fear of uncertainty and the potential for negative outcomes.
Traditional OCD Examples
- Contamination Fears: Lisa washes her hands excessively and avoids public places to prevent contamination from germs, even in situations with minimal risk.
- Fear of Harm: John checks the stove multiple times before leaving the house, worried he might cause a fire, despite no evidence suggesting he left it on.
- Not Just Right Experiences: Anne arranges her books repeatedly until they feel “just right,” a process that can take hours and interferes with her daily life.
- Checking and Reassurances: David repeatedly asks his family if they are sure the doors are locked, needing constant reassurance to alleviate his fears.
- Fear of Self: Maria avoids knives and sharp objects, fearing she might lose control and harm someone, despite having no history of violence.
Comparison
In Pure O OCD, the struggles are largely internal. The distress is caused by intrusive thoughts, the need for certainty, and mental rituals. These individuals might appear untroubled on the outside, but they are often engaged in a constant internal battle with their thoughts.
In contrast, traditional OCD is characterized by visible compulsions, such as cleaning, checking, or arranging objects, driven by fears of contamination, harm, or a need for things to be just right. These compulsions are often noticeable and can significantly disrupt daily life.
Both forms of OCD involve significant distress and impairment, but the nature of that distress differs. Understanding these differences is crucial for effective diagnosis and treatment. In the final part of the article, we will summarize these differences and discuss the importance of recognizing these distinct manifestations of OCD.
How OCD and Pure O OCD manifest in real-life situations
Here’s a table comparing how OCD and Pure O OCD manifest in real-life situations for two individuals, Sarah (with Pure O OCD) and Kai (with traditional OCD):
| Situation | Sarah (Pure O OCD) | Kai (Traditional OCD) |
|---|---|---|
| Morning Routine | Spends hours ruminating over whether she turned off the appliances, despite no evidence of forgetting. | Repeatedly checks locks, appliances, and windows before leaving home, consuming a lot of time. |
| Work Environment | Constantly doubts the quality of her work and seeks reassurance, leading to reduced productivity. | Organizes and reorganizes his workspace compulsively, finding it hard to focus if things aren’t ‘just right’. |
| Social Interaction | Avoids social gatherings due to fear of having intrusive thoughts about harming others. | Frequently washes hands and avoids physical contact, fearing contamination. |
| Leisure Time | Struggles to relax as she is preoccupied with intrusive thoughts and mental rituals to neutralize them. | Spends leisure time engaging in compulsive behaviors like cleaning or checking. |
| Decision Making | Has difficulty making decisions, fearing that the wrong choice could lead to disastrous outcomes. | Seeks repeated reassurance from others before making decisions, fearing the consequences of mistakes. |
| Reacting to Stress | Experiences heightened anxiety and engages in mental rituals to cope with stress. | Under stress, resorts to increased checking, cleaning, or other compulsive behaviors. |
This table illustrates how Sarah’s Pure O OCD primarily manifests in internal struggles like rumination and mental rituals, while Kai’s traditional OCD is characterized by visible compulsive behaviors.

Conclusion: Navigating the Distinctive Realms of OCD and Pure O OCD
In this exploration of OCD and Pure O OCD, we have delved into the unique cognitive themes that characterize each condition. While both disorders share the common thread of anxiety and distress caused by intrusive thoughts, their manifestations and impacts on individuals’ lives are distinctly different.
Key Takeaways:
- Nature of Symptoms: Traditional OCD is marked by observable compulsions, such as excessive cleaning or checking, driven by fears like contamination or harm. Pure O OCD, in contrast, is characterized by internal struggles, where compulsions are mental and less visible, such as mental rituals and excessive analysis.
- Internal vs. External Battles: Pure O OCD is a battle waged internally, with sufferers grappling with intrusive thoughts, the need for certainty, and fear of acting on these thoughts. Traditional OCD involves more external battles, where the individual engages in visible behaviors to alleviate anxiety.
- Understanding for Treatment: Recognizing these differences is vital for effective treatment. Pure O OCD may require approaches focusing on managing intrusive thoughts and reducing mental rituals, whereas traditional OCD treatment might focus more on exposure and response prevention to address visible compulsions.
- Compassion and Awareness: Both forms of OCD can be deeply distressing and debilitating. Greater awareness and understanding of these conditions are essential for fostering compassion and providing appropriate support to those affected.
In conclusion, OCD, whether in its traditional form or as Pure O OCD, presents significant challenges to those who experience it. By understanding the nuanced differences in their cognitive themes and manifestations, we can better support individuals in managing their symptoms and improving their quality of life. This exploration underscores the importance of tailored approaches in mental health treatment and the need for ongoing research and awareness to aid those living with these complex conditions.