Body dysmorphia and OCD are complex mental health challenges that manifest through appearance obsessions, mirror checking, and grooming compulsions. This article explores these topics using a cognitive-behavioral therapy (CBT) approach to elucidate the connection between maladaptive beliefs, thinking patterns, and emotional responses, ultimately leading to improved mental wellbeing.
The Nature of Body Dysmorphic Disorder
Body Dysmorphic Disorder (BDD) is a mental health condition characterized by an obsessive focus on perceived flaws in appearance, which are often minor or nonexistent. The profound nature of this disorder can significantly impact an individual’s daily life, self-esteem, and relationships. Research indicates that the prevalence of BDD ranges from 1% to 2% of the population, although it may be underestimated due to the stigma surrounding mental health issues. Those affected often feel isolated, ashamed, and misunderstood, largely due to the erroneous belief that others are constantly judging their appearance.
Individuals with BDD experience various symptoms, which may include compulsively checking mirrors, seeking reassurance from others, or avoiding mirrors altogether. These rituals often become time-consuming. A person may spend hours getting ready for the day, scrutinizing themselves in every reflective surface, from car windows to bathroom mirrors. This excessive grooming is a way to attempt to fix the perceived flaws but can, paradoxically, lead to increased distress. The cognitive distortions central to BDD contribute to the cycle of obsession and compulsion. Many individuals harbor a skewed body image, leading them to focus obsessively on specific features, such as their skin, hair, or weight. This preoccupation can create a false sense of reality, where the individual believes that others perceive them as flawed or unattractive.
The relationship between BDD and cognitive distortion is significant. Cognitive distortions are negative thought patterns that reinforce feelings of inadequacy and self-criticism. For example, a person might have a thought like, “If I don’t look perfect today, everyone will notice, and they’ll think I’m ugly.” Such thoughts can lead to spirals of shame and sadness. Individuals struggling with BDD often succumb to “all or nothing” thinking; they may believe that unless they attain a certain beauty standard, their worth is diminished. To illustrate, consider Sarah, a 25-year-old woman with BDD. She may spend large portions of her day meticulously applying makeup, checking her reflection, and posting photos on social media in the hopes of receiving validation. Despite numerous compliments, Sarah’s internal dialogue convinces her that she is not beautiful, fueling her quest to change her appearance.
The impact of BDD on daily functioning can be debilitating. Individuals may avoid social situations, leading to isolation. For instance, Jake, a 30-year-old man, feels uncomfortable engaging with friends because he fears they will judge him for his perceived skin flaws. This avoidance can lead to a downward spiral, where the lack of social interaction exacerbates feelings of loneliness and depression. Additionally, BDD can affect career choices; some may avoid positions involving public interaction or visibility, limiting personal and professional growth.
Beyond the individual experience, the harmful effects of BDD extend to relationships, affecting how individuals connect with family, friends, and romantic partners. The need for constant reassurance can strain relationships, as loved ones may feel helpless or frustrated in their attempts to support the individual. Furthermore, the embarrassment of living with a mental health disorder can alienate individuals from their support networks, compounding the challenge of recovery.
Cognitive-behavioral therapy (CBT) has emerged as an effective treatment for BDD, helping individuals reframe negative thoughts and reduce harmful behaviors. By challenging cognitive distortions and gradually confronting feared situations, individuals can begin to cultivate a healthier relationship with their body image and ultimately, themselves. Understanding the pervasive nature of BDD, from its symptoms to its debilitating impact, is the first step toward empathy and support for those affected, as well as for the professionals who seek to assist them. The path to healing is complex and often requires a multifaceted approach that emphasizes both mental wellbeing and resilience.
Obsessive-Compulsive Disorder and Appearance Obsessions
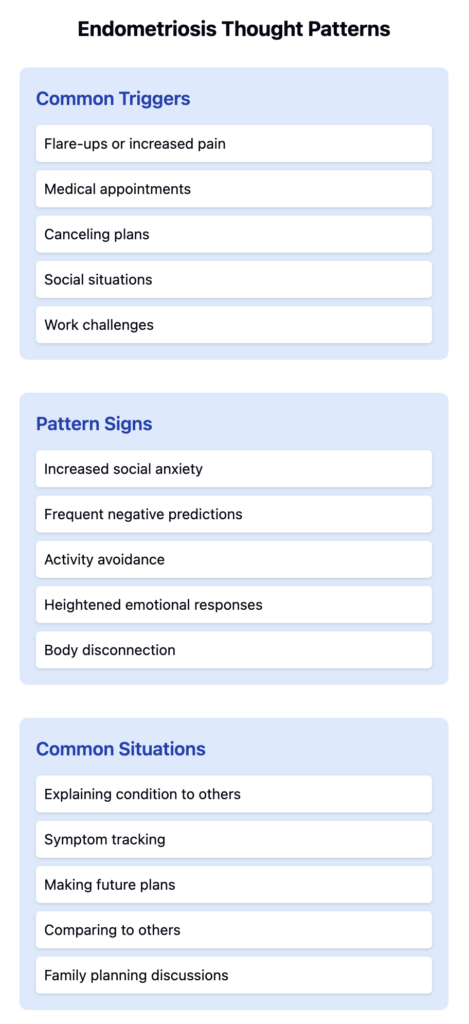
Obsessive-compulsive disorder (OCD) is a mental health condition characterized by persistent, intrusive thoughts and repetitive behaviors that individuals feel compelled to perform. When it comes to appearance obsessions, OCD manifests through excessive concern over perceived imperfections in one’s appearance, often leading to maladaptive behaviors that further entrench the cycle of anxiety and self-criticism. The connection between OCD and body image issues is profound, revealing the intricate ways in which cognitive patterns shape an individual’s self-perception and overall mental wellbeing.
Individuals dealing with body image OCD frequently experience a barrage of intrusive thoughts that trigger feelings of inadequacy or dysphoria. These thoughts can range from minor insecurities to overwhelming fears about looking unattractive, unkempt, or flawed in some way. For instance, someone might find themselves preoccupied with thoughts like, “What if people notice this blemish?” or “Am I the only one who thinks my nose is too big?” Such cognitive distortions not only fuel anxiety but also provoke a multitude of compulsions aimed at neutralizing these distressing thoughts.
Mirror checking is one of the hallmark compulsions associated with body image OCD. Individuals feel an urgent need to repeatedly assess their appearance in mirrors, often scrutinizing specific features they perceive as problematic. This evaluation can become a time-consuming ritual, where hours are spent checking reflections, adjusting hair, or attempting to conceal perceived flaws with makeup or clothing. Unfortunately, while this behavior may provide temporary relief, it ultimately reinforces the same intrusive thoughts, causing a vicious cycle where individuals become trapped in an endless quest for reassurance.
Grooming compulsions further illustrate how deeply ingrained appearance obsessions can affect daily functionality. People might engage in excessive grooming rituals, such as frequent hair styling, skin treatments, or even cosmetic procedures, in an effort to attain an unattainable standard of appearance. While grooming can be a normal part of self-care, in the context of body image OCD, it transitions from a healthy practice to a compulsive behavior. This shift often leads to feelings of shame and frustration as individuals recognize that their grooming habits are excessive yet feel powerless to stop.
Moreover, it’s pivotal to understand that the compulsive nature of these behaviors is often a misguided attempt to combat the crippling anxiety brought on by intrusive thoughts. Each compulsive act provides a fleeting sense of control or temporary alleviation of discomfort, leading individuals to firmly believe that without such rituals, they will be unable to manage their distress. This disastrous cycle perpetuates a heightened focus on appearance, detracting from a holistic sense of self-worth and exacerbating the very symptoms they are attempting to mitigate.
To illustrate the detrimental effects of appearance obsessions, consider the case of Emily, a 28-year-old who began developing OCD symptoms in her late teens. She finds herself consumed by thoughts about the thickness of her thighs; every time she passes a reflective surface, she experiences a panic attack, scrutinizing her body to seek validation or assurance. Emily started avoiding situations where she would have to wear shorts or skirts, opting for clothing that hides her legs, limiting her social engagements and deepening her feelings of isolation. Each act of avoidance only solidifies her fears, reinforcing the belief that her appearance is unacceptable and driving her deeper into compulsive behavior.
Understanding these patterns sheds light on the critical need to distinguish between the reality of one’s appearance and the cognitive distortions influencing perception. This approach highlights the necessity for empathy and support in navigating the complexities of body image OCD. By recognizing that these obsessions and compulsions are often rooted in deeper cognitive processes, care providers can facilitate more comprehensive treatment, leading individuals toward understanding the disconnect between their thoughts and their intrinsic value. In doing so, there’s an opportunity for growth and recovery that transcends mere appearance, focusing instead on the individual’s journey toward acceptance and resilience.
Transforming Thoughts with Cognitive Behavioral Therapy
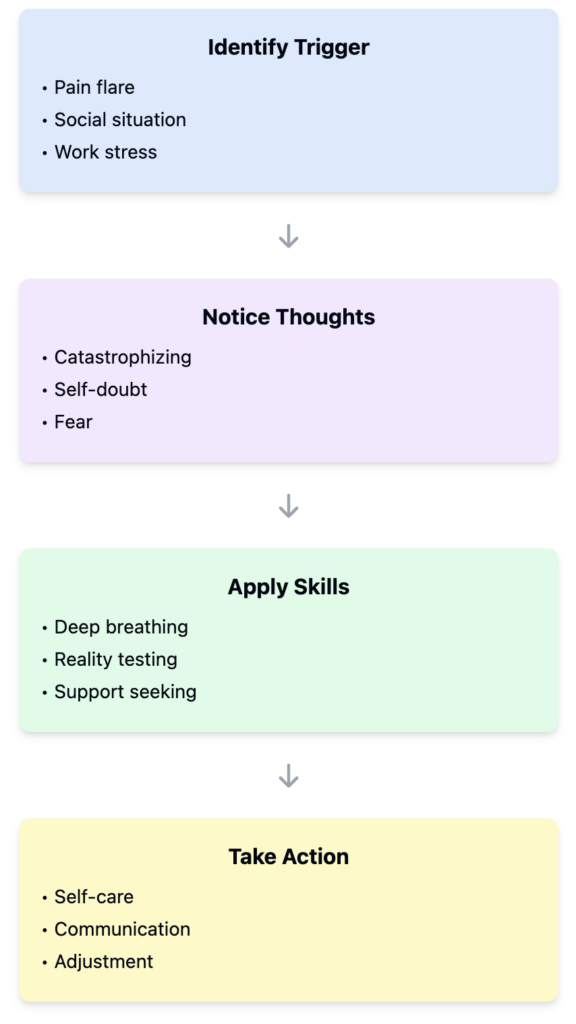
Cognitive-Behavioral Therapy (CBT) offers a valuable framework for understanding and treating body dysmorphia and its intersection with obsessive-compulsive disorder (OCD). By addressing the distorted beliefs and maladaptive thought patterns that drive the excessive preoccupation with appearance, CBT empowers individuals to reclaim their emotional wellbeing. Understanding how to transform these thoughts forms the cornerstone of effective treatment.
At the core of body dysmorphic disorder (BDD) is a fixation on specific perceived flaws in one’s appearance, which are often minor or nonexistent. Individuals with BDD frequently engage in mirror checking, repeatedly evaluating their reflection for reassurance. This behavior feeds the cycle of obsession, leading to increased anxiety and setting the stage for compulsive grooming rituals aimed at rectifying perceived imperfections. Through CBT, clients learn to recognize how their thoughts influence feelings about themselves, thereby dismantling the hold these intrusive ideas have over their actions and emotions.
For instance, consider Sarah, a 28-year-old woman who has long struggled with BDD. Her day begins with extensive time spent in front of the mirror, obsessively scrutinizing her skin for perceived blemishes. This ritual consumes her mornings, often leading to tardiness at work and damaged relationships with her peers. In therapy, Sarah learns to confront the thoughts behind her mirror checks. What do these actions say about her self-worth? Together with her therapist, she identifies the maladaptive belief that her appearance is directly tied to her value as a person.
Over time, Sarah adopts new cognitive strategies to replace her harmful thoughts. Instead of affirming her worth is contingent upon her looks, she begins practicing self-compassion. Using CBT techniques such as cognitive restructuring, Sarah learns to challenge her negative thoughts by asking herself whether they are factual or helpful. When that persistent inner voice insists that a tiny mark on her face makes her “ugly,” she reframes it, reminding herself of moments she radiated joy and confidence, irrespective of her appearance.
In CBT, exposure therapy is another critical component that complements cognitive restructuring. Sarah’s therapist encourages her to gradually reduce mirror checking. Initially, they set small achievable goals, like delaying her first mirror check by five minutes each day. As Sarah builds her tolerance to discomfort, she realizes her thoughts do not dictate her reality. Gradually, she becomes less reliant on external validation for her self-esteem.
The success of CBT also hinges on clients understanding the connection between beliefs, thinking, and feelings. Cognitive distortions, such as “catastrophizing” or “black-and-white thinking,” can exacerbate body image concerns. Treatment focuses on identifying these thought patterns and replacing them with more nuanced and flexible thinking. For example, a thought like “If I don’t look perfect, nobody will love me” can be reframed as “People who care about me appreciate my character and personality, not just my looks.”
Another client, Mark, experienced grooming compulsions that intertwined with his BDD. He would spend hours grooming to mitigate feelings of inadequacy about his hair. Through CBT, he learns mindfulness techniques that help him engage with his thoughts without judgment. Instead of succumbing to the compulsion to groom, he practices moment-to-moment awareness, absorbing the sensations around him, leading to a significant reduction in anxiety.
Case studies illustrate that while the journey through CBT may be challenging, the transformation of one’s thinking is profound. As clients learn to disentangle their self-worth from their appearance, not only do symptoms decline, but emotional resilience is also fostered. By fostering a therapeutic environment that emphasizes empathy and understanding, CBT offers an effective pathway toward healthier self-perception, promoting lasting change.
Through consistent application of these strategies and insights, individuals struggling with body dysmorphia can find hope and healing, paving the way for a future where their identity transcends appearance, leading to a more fulfilling and connected life.
Conclusions
In conclusion, addressing body dysmorphia and OCD through a CBT framework allows individuals to reshape their beliefs, enhance their emotional resilience, and reduce symptoms. By mapping these thought processes and promoting flexible thinking, we can foster a healthier self-image and improved mental wellbeing.