Obsessive-Compulsive Disorder (OCD) can be isolating, but connecting with support groups and online communities offers significant assistance. This article explores how Cognitive Behavioral Therapy (CBT) methods are reinforced through shared experiences and peer support, enhancing our understanding of maladaptive beliefs, and building emotional resilience.
Understanding OCD and Its Challenges
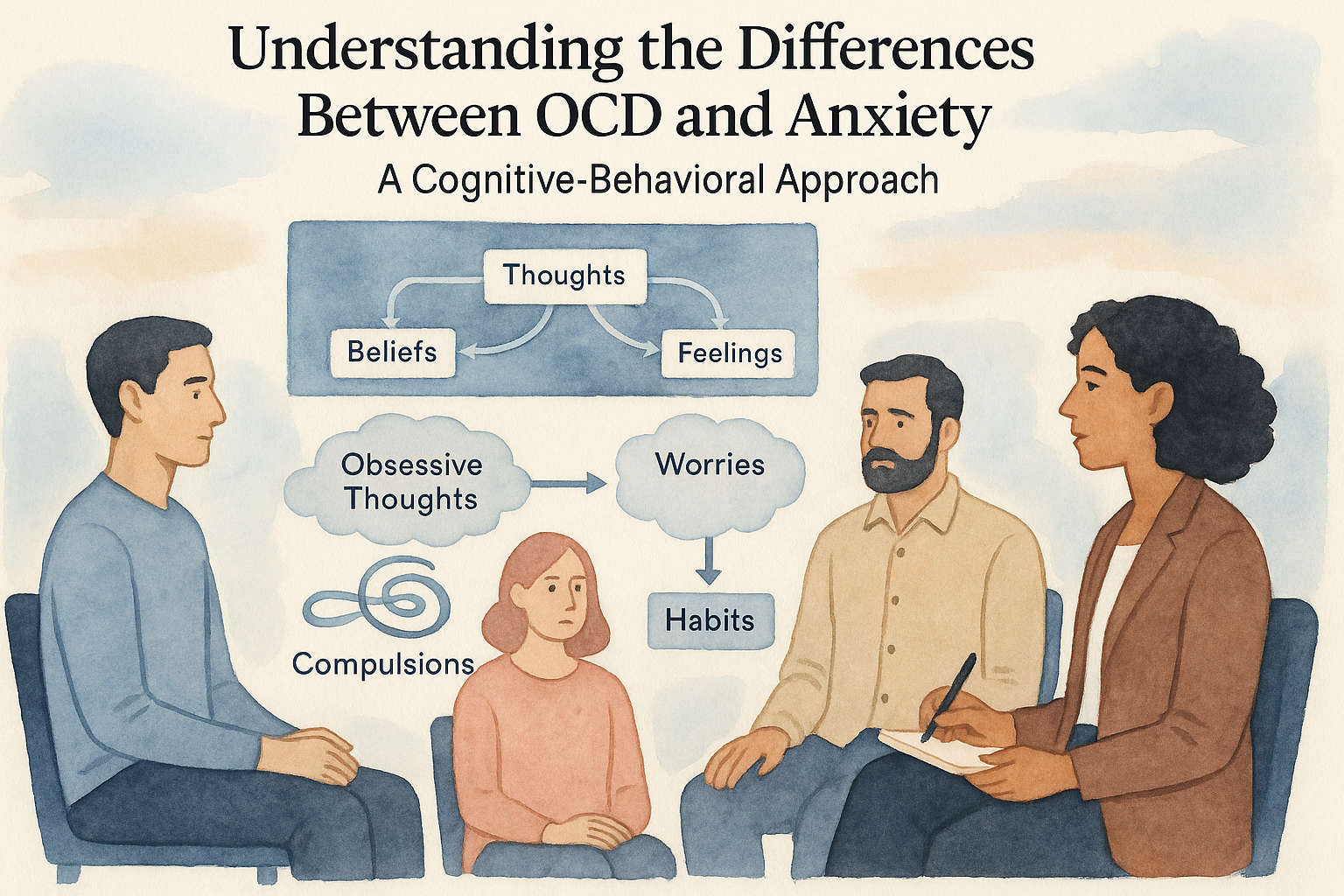
Obsessive-Compulsive Disorder (OCD) is a mental health condition characterized by persistent, unwanted thoughts, known as obsessions, and repetitive behaviors or mental acts, referred to as compulsions. Individuals with OCD may experience obsessions that fuel anxiety, leading them to engage in compulsive actions as a form of temporary relief. For example, a person might obsessively worry about germs, prompting them to wash their hands repeatedly, far beyond what is deemed necessary. This cycle of obsession and compulsion can severely impact daily functioning, relationships, and overall quality of life.
Statistically, OCD affects approximately 1-2% of the global population, with many individuals experiencing symptoms during childhood or adolescence. The emotional toll is significant, as those living with OCD often feel isolated, misunderstood, and anxious. Many individuals harbor maladaptive beliefs, such as a fear of losing control or a need for certainty, which exacerbate their compulsive behaviors. Through narratives, one can glean the intricacies of OCD; for instance, consider someone eternally trapped in a ritual of double-checking locks and appliances because the mere thought of leaving them unattended sparks immense dread—an internal battle diminishing both time and peace of mind.
As those with OCD navigate these challenges, connecting with others becomes vital. Support groups offer a safe haven for individuals to share their experiences, fears, and triumphs. The power of community lies in its ability to foster understanding and reduce feelings of isolation. Local support groups, often facilitated by mental health professionals, create a space for participants to discuss their struggles openly. Here, members discover they are not alone in their experiences, and share practical strategies for managing symptoms. These face-to-face interactions allow for real-time feedback and support, fostering a sense of belonging that is often elusive to individuals with OCD.
In addition to local gatherings, the rise of online forums has opened avenues for connection that transcend geographical limitations. International online communities serve a crucial role, particularly for those who may feel hesitant to attend in-person meetings or lack access to local resources. Through platforms dedicated to mental health, individuals can anonymously share their stories, ask for guidance, and seek solace in knowing that others are experiencing similar challenges. Online forums not only provide peer support but also promote the sharing of evidence-based practices in managing OCD.
Peer support is pivotal in reinforcing resilience. Members share coping strategies grounded in Cognitive Behavioral Therapy (CBT)—a widely recognized treatment for OCD. By engaging with others who have traversed similar paths, individuals can learn about exposure and response prevention (ERP) techniques that allow them to confront their compulsions while refraining from performing ritualistic behaviors. This collective learning journey strengthens adherence to therapeutic practices, as members encourage one another to take those crucial first steps toward facing their fears.
Families play an equally important role in the support ecosystem for individuals with OCD. Education for family members about OCD can demystify the condition, allowing loved ones to become more empathetic and supportive. Family members armed with knowledge can help create an environment that fosters healthy communication and reduces enabling behaviors that might inadvertently feed the disorder.
Ultimately, the journey through OCD may be inherently challenging, but the presence of a supportive community acts as a beacon of hope. Individuals navigating OCD can find solace not only in the shared experiences of others but also in the understanding and encouragement that thrives within these communities. This network of support not only alleviates the burden but empowers individuals to reclaim their lives, bolstered by the knowledge that they are not facing their struggles in isolation.
The Healing Power of Community Support
Individuals navigating the complexities of Obsessive-Compulsive Disorder (OCD) often find themselves trapped in a cycle of isolation, exacerbated by the nature of their symptoms. In this challenging context, support groups, both local and online, emerge as lifelines, offering safe spaces where those wrestling with similar struggles can gather, share experiences, and cultivate connections. The healing power of community support lies in its ability to foster understanding, diminish feelings of loneliness, and instill hope as members embark on the path toward mental wellness.
Support groups can manifest in various formats. Local support groups provide face-to-face interaction, enabling members to engage in meaningful discussions about their experiences with OCD, coping strategies, and the intricacies of living with the disorder. These gatherings often serve as practical extensions of Cognitive Behavioral Therapy (CBT) principles, where individuals practice exposure tasks within a supportive environment, learning that they are not alone in their struggles. Participants share their journeys, illustrating both their challenges and progression, thus helping others identify that recovery is indeed possible.
In today’s digital age, online forums offer another avenue for community connection, transcending geographical barriers. These platforms can include private Facebook groups, specialized websites, and forums dedicated to OCD. Not only do they allow individuals to remain anonymous—reducing the fear of judgment—they also enable access to a global network of support. Through shared experiences in these online settings, members can witness a range of coping mechanisms and therapeutic strategies. Insights gleaned from international perspectives add richness to the dialogue, broadening understanding and approaches to OCD management across cultural contexts.
Many firsthand accounts illustrate the transformative nature of these communities. Sarah, a young adult diagnosed with OCD, describes how joining a local support group illuminated her path to recovery. Initially hesitant, Sarah attended her first meeting after experiencing overwhelming isolation. There, she discovered others who understood her compulsions—discussions about intrusive thoughts resonated deep within her. The friendships formed in that group provided her with a consistent support network, empowering her to confront her OCD with newfound resilience. “I realized I wasn’t alone,” she remarks, emphasizing the role of community in her coping strategy; she learned that sharing her experiences helped dismantle the power of her obsessions.
Online forums have equally impactful stories. For Jonathan, a college student managing severe OCD, an online platform became an essential space for expression and encouragement. He recalls nights spent reading others’ posts detailing their OCD struggles and triumphs. The connections formed through replies and comments provided Jonathan with insights into cognitive restructuring techniques he hadn’t tried yet, drawn from the principles of CBT. “It was like a community of warriors fighting the same battle,” he explains, highlighting the camaraderie that alleviated his sense of isolation.
Beyond support groups and online forums, family education and involvement are pivotal in amplifying the positive impact of community. By fostering understanding of OCD through workshops and informational sessions, families can become integral components of their loved ones’ lives. An informed family can help create an environment that supports exposure tasks, providing encouragement without judgment. This integration of family dynamics with community support not only enhances the individual’s resilience but also promotes a collective approach to tackling the barriers posed by the disorder. With family members armed with knowledge and empathy, the overall treatment experience becomes more holistic and reassuring for everyone involved.
Ultimately, the healing power of community support for individuals with OCD cannot be underestimated. Whether through local support groups or expansive online networks, the connections made within these communities spotlight shared experiences, reduce the emotional burden of isolation, and underscore the fundamental truth: recovery is a journey best undertaken together.
Peer Support and Advanced Education for Families
Peer support and family education play a crucial role in managing Obsessive-Compulsive Disorder (OCD) by fostering understanding, empathy, and effective coping strategies. For individuals grappling with OCD, the presence of informed and supportive family members can significantly enhance their journey toward recovery and resilience.
Understanding OCD is essential for families, as it allows them to provide meaningful support. Families often benefit from educational resources that explain the nature of OCD, its symptoms, and its impact on daily life. This knowledge helps to dispel misconceptions and reduces feelings of frustration or helplessness that family members may experience. Providing education through workshops, literature, or therapist-led sessions can greatly empower families to become allies in their loved one’s journey.
Empathy is at the heart of effective family support. It is vital for family members to approach their loved ones’ struggles with sensitivity and understanding, recognizing that OCD is a mental health condition and not a personal failing. When families cultivate empathy, they create an environment where individuals feel safe to express their thoughts and anxieties without fear of judgment. This improved communication facilitates a healthier atmosphere for discussing challenges, triggers, and coping mechanisms.
Another effective strategy includes actively involving family members in therapy sessions. When families attend therapy alongside their loved ones, they gain firsthand insight into therapeutic techniques, such as Cognitive Behavioral Therapy (CBT) strategies tailored to treating OCD. This shared space fosters collaboration, allowing families to practice supportive communication while reinforcing skills learned in therapy. Moreover, participating in therapy together can help reduce feelings of isolation and helplessness among family members, as they better understand what their loved ones experience.
Family roles in supporting an individual with OCD can vary, but certain practices are universally beneficial. One effective communication method is to use “I” statements. Instead of saying “You need to stop your compulsions,” a family member might say, “I feel concerned when I see you distressed.” This technique emphasizes feelings and concerns rather than placing blame, helping to foster productive dialogue. Encouragement is also vital; celebrating small victories can bolster an individual’s sense of achievement and motivation within their recovery journey.
Families can also educate themselves about exposure and response prevention, a form of CBT designed specifically for OCD. Understanding the rationale behind gradual exposure to feared stimuli and resisting compulsions can empower family members to provide appropriate support. For instance, during exposure tasks, family members might help by offering encouragement and refraining from participating in compulsive behaviors themselves, promoting an environment of healthy resistance.
Support doesn’t solely come from educated family members; peer support groups create invaluable spaces for sharing experiences and advice. Family members can engage in support groups specifically tailored for loved ones of individuals with OCD. These groups foster a sense of community, allowing families to discuss challenges and share strategies, thereby alleviating feelings of isolation and confusion. Additionally, connecting with other relatives who share similar experiences can cultivate hope and resilience for both the individual with OCD and their support network.
Incorporating CBT principles into family education ensures that family members are equipped not just to provide emotional support, but also to assist in challenging maladaptive thoughts associated with OCD. When families understand how to navigate moments of crisis with appropriate responses—like practicing exposure tasks or employing cognitive restructuring techniques—they can help create a supportive environment that actively promotes recovery.
Engaging in open communication and education about OCD enables families to become effective advocates for their loved ones. With empathy, education, and the encouragement of positive coping strategies, families can significantly influence an individual’s ability to cope with OCD, fostering a journey marked by resilience and hope.
Shifting Beliefs Through Cognitive Behavioral Therapy
As individuals confront the overwhelming challenges associated with Obsessive-Compulsive Disorder (OCD), the role of Cognitive Behavioral Therapy (CBT) becomes pivotal in reframing their understanding and reactions to intrusive thoughts and compulsions. By effectively implementing CBT techniques, individuals can learn to identify and shift maladaptive beliefs that exacerbate the distress caused by OCD, facilitating a path toward resilience and recovery.
CBT emphasizes the connection between thoughts, feelings, and behaviors, making it an effective approach for addressing the cognitive distortions prevalent in OCD. For instance, a common belief in individuals with OCD is that having a certain thought means they are somehow responsible for an unwanted outcome. This belief can lead to compulsive behaviors aimed at “neutralizing” those thoughts. Through cognitive restructuring techniques used in CBT, individuals can learn to challenge and modify such beliefs.
A practical method in this process is **thought records**, where individuals track their obsessions and analyze the accuracy and outcomes of their beliefs. For instance, someone who fears that thinking about a loved one’s safety could bring about harm might write down this thought, rate the anxiety it causes, and then look for evidence against it. Often, upon examining the situation closely, individuals can see that their thoughts lack a factual basis. This realization can lessen the grip of compulsions over time, highlighting the transformative power of adaptive thinking.
Consider the example of Sarah, who struggled with contamination fears tied to OCD. Initially, her belief was that touching anything perceived as “dirty” would lead to illness or harm to her loved ones. In therapy, Sarah learned to challenge this belief through exposure exercises and cognitive restructuring. By gradually confronting her fears in a controlled manner, she noted the absence of negative outcomes and began to reduce her compulsive hand-washing behaviors. The community support she received from an OCD support group was invaluable during this journey, as members shared their experiences and strategies for coping with similar challenges.
The role of community cannot be overstated, as shared experiences foster a sense of belonging and understanding. Individuals attending support groups often hear narratives that mirror their own, which helps to validate their feelings and beliefs. Such connections can serve as a powerful reminder that they are not alone in their struggles. When someone in a support group reframes a negative belief, it can resonate with others, creating an opportunity for collective growth.
Family education plays a complementary role in this cognitive transformation. When family members understand the principles of CBT and the importance of challenging maladaptive thoughts, they can more effectively support their loved ones. For instance, they might engage in discussions about cognitive distortions without judgment, helping individuals recognize patterns and apply CBT techniques outside of therapy. This collaboration reinforces the newly adopted adaptive beliefs, enabling individuals to feel more secure in their recovery process.
Online forums and virtual peer support groups also provide another layer of accessibility and community for individuals facing OCD. These platforms allow individuals to share their victories, no matter how small, and seek advice during setbacks. The instant feedback and collective wisdom found in these spaces can aid individuals in practice and encourage the application of CBT strategies such as thought challenging, thereby strengthening resilience.
Ultimately, the interplay between community support and cognitive restructuring amplifies the benefits of CBT for OCD. By surrounding oneself with empathetic peers and educated family members, individuals are better equipped to confront their fears and transform their belief systems. The journey toward mental wellness is profoundly influenced not only by individual effort but also by the supportive network that reinforces adaptive thoughts and behaviors, enabling sustained resilience against the nuances of OCD. In this collaborative environment, the principles of CBT come alive, paving the way for lasting change and improved mental wellness.
Conclusions
In summary, embracing peer support and cognitive principles can transform the way individuals manage OCD. By re-evaluating beliefs and fostering community connections, those affected can cultivate emotional strength and well-being, illustrating the profound impact of shared experiences and supportive networks.