Living with endometriosis involves managing not just physical symptoms, but also significant psychological challenges. As a chronic condition affecting approximately 10% of reproductive-age women, endometriosis can profoundly impact mental well-being in ways that often go unaddressed in traditional medical care.
The relationship between physical symptoms and psychological distress in endometriosis is complex and bidirectional. Chronic pain and uncertainty about symptoms can trigger negative thought patterns, while these thought patterns can, in turn, influence how we experience and cope with physical symptoms. Research has shown that women with endometriosis often experience higher rates of anxiety and depression compared to those without the condition, making it crucial to address both the physical and psychological aspects of the disease.
This article aims to help you understand common maladaptive thinking patterns that may develop when living with endometriosis, and more importantly, how to recognize and challenge these thoughts using evidence-based approaches. By understanding these patterns, you can develop more adaptive ways of thinking about your condition while maintaining hope and agency in your journey.
Let’s understand these patterns and learn practical strategies for managing them effectively, drawing from cognitive behavioral therapy (CBT) principles that have shown significant benefits for women with chronic health conditions.
Understanding Maladaptive Thinking Patterns
When living with endometriosis, certain thought patterns may develop as we try to make sense of our experiences. These patterns, while understandable, can sometimes work against our well-being. Let’s examine each pattern in detail:
A. Pain-Related Catastrophizing Catastrophic thinking about pain often manifests as assuming the worst possible outcomes. You might find yourself thinking “This pain will never end” or “Something must be terribly wrong.” While pain is real and valid, catastrophizing can amplify our distress and potentially increase pain sensitivity.
B. Body Betrayal and Mistrust Many women with endometriosis develop a complex relationship with their bodies, often feeling betrayed or unable to trust their physical experiences. Thoughts like “My body is working against me” or “I can’t trust my own body” are common. This disconnect can affect how we care for ourselves and make health decisions.
C. Self-Worth and Identity Challenges Endometriosis can impact how we view ourselves and our worth. Thoughts like “I’m less of a woman” or “I’m a burden to others” may arise. These beliefs often stem from societal pressures and misconceptions about chronic illness, rather than reflecting reality.
D. Social and Relationship Concerns The invisible nature of endometriosis can lead to thoughts about being misunderstood or isolated. You might think “No one understands what I’m going through” or worry about maintaining relationships. These thoughts can influence how we interact with others and seek support.
E. Control and Uncertainty Issues Living with a chronic condition involves managing uncertainty. Thoughts like “I have no control over my life” or “I can’t plan anything” are common responses to the unpredictable nature of symptoms.
Understanding these patterns is the first step toward developing a healthier relationship with our thoughts. Remember, having these thoughts doesn’t mean you’re doing anything wrong – they’re common responses to managing a chronic condition.
Recognizing Your Thought Patterns
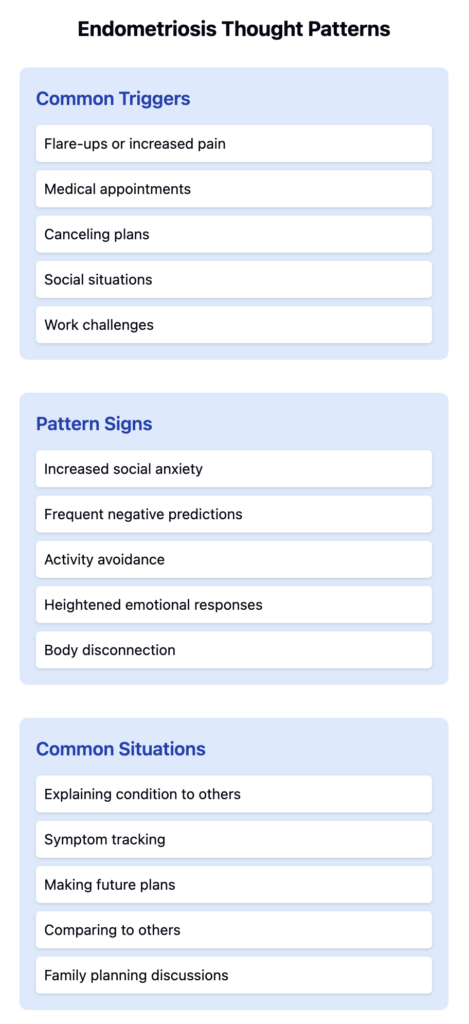
These maladaptive thought patterns often emerge in specific situations or in response to particular triggers. Learning to recognize them in real-time is essential for developing better coping strategies.
Common Triggers:
- Flare-ups or increased pain intensity
- Medical appointments or procedures
- Having to cancel plans due to symptoms
- Intimate relationships or social situations
- Work-related challenges or accommodations
Signs You’re Experiencing These Patterns:
- Noticing increased anxiety before or during social events
- Finding yourself frequently predicting negative outcomes
- Avoiding activities or connections due to fear of symptoms
- Experiencing heightened emotional responses to physical symptoms
- Feeling disconnected from your body during pain episodes
Common Situations Where These Thoughts Arise:
- When explaining your condition to others
- During symptom tracking or health monitoring
- While making future plans or commitments
- When comparing your experiences to others
- During conversations about fertility or family planning
Pay attention to your internal dialogue during these moments. Consider keeping a thought journal to track patterns and identify specific triggers that consistently lead to maladaptive thinking.
The Impact on Daily Life
Living with endometriosis-related thought patterns can significantly affect various aspects of life:
Daily Activities
- Avoiding social events due to symptom anticipation
- Reduced participation in physical activities
- Difficulty maintaining regular work schedules
- Postponing important decisions
Pain Management
- Increased pain sensitivity due to anxiety
- Reduced effectiveness of pain management strategies
- Hesitation to try new treatments
- Over-focusing on symptoms
Relationships
- Difficulty discussing symptoms with partners
- Withdrawing from social connections
- Reduced intimacy due to anxiety
- Hesitation to form new relationships
Professional Impact
- Reluctance to seek accommodations
- Career decisions based on worst-case scenarios
- Increased stress about job security
- Difficulty setting professional boundaries
The cycle between thoughts and symptoms:
- Negative thoughts increase stress
- Stress can amplify physical symptoms
- Worsened symptoms reinforce negative thoughts
- This cycle affects both mental and physical well-being
These impacts are not permanent – recognizing them is the first step toward developing healthier coping strategies.
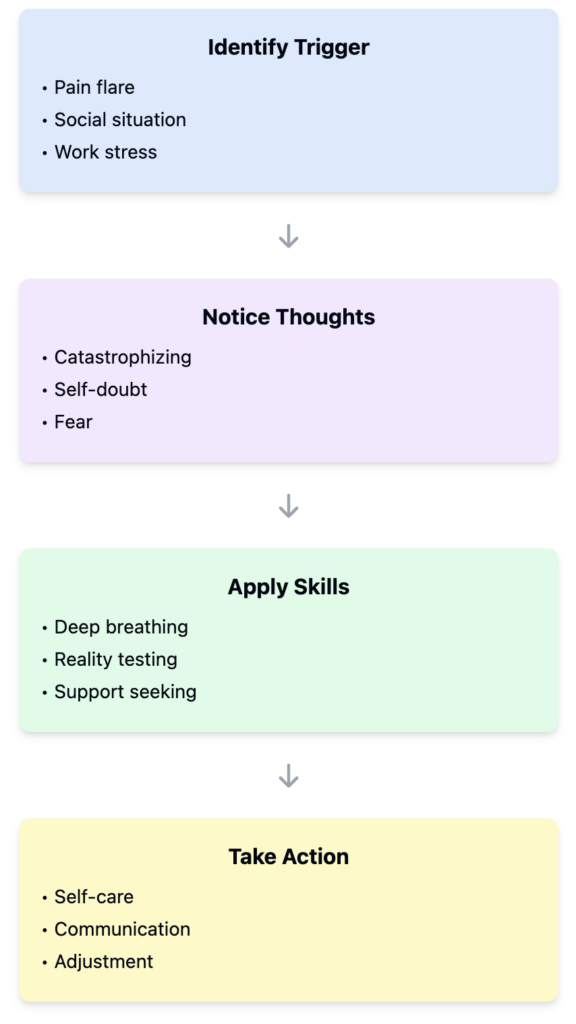
Challenging Thinking Patterns
Evidence-Based Strategies:
- Cognitive Restructuring
- Identify the thought: “I’ll never manage this pain”
- Examine evidence for and against
- Develop balanced perspective: “I have managed flares before and have support systems”
- Behavioral Techniques
- Gradual exposure to avoided activities
- Setting achievable daily goals
- Maintaining routine despite symptoms
- Recording successful coping instances
- Self-Compassion Practices
- Acknowledging difficulty without judgment
- Treating yourself with same kindness as others
- Recognizing shared experiences with other patients
- CBT-Based Tools
- Thought records tracking triggers and responses
- Pain management diaries
- Graded activity planning
- Relaxation techniques
- Communication Strategies
- Clear expression of needs
- Setting boundaries
- Educating others about condition
- Building support network
Each strategy should be practiced consistently and adjusted based on individual needs and responses.
VI. Building Resilience
Developing resilience while living with endometriosis requires a balanced approach that acknowledges both challenges and opportunities for growth. Let’s explore key strategies that can help strengthen your ability to cope with daily challenges.
Developing Healthier Thought Patterns
Resilience starts with reshaping how we think about our experiences. Rather than aiming for constant positivity, focus on realistic optimism. When symptoms flare, remind yourself of past instances where you’ve successfully managed similar situations. Notice when catastrophic thinking appears (“I’ll never feel better”) and practice replacing it with more balanced thoughts (“This is difficult right now, but I have strategies to cope”).
Creating Support Systems
Building resilience isn’t a solo journey. Start by identifying healthcare providers who listen to and validate your experiences. Consider connecting with endometriosis support groups, either locally or online, where you can share experiences with others who truly understand. When choosing confidants among friends and family, look for those who demonstrate empathy and willingness to learn about your condition. Professional mental health support, particularly from therapists familiar with chronic health conditions, can provide additional tools for managing both physical and emotional challenges.
Setting Realistic Goals
Goal-setting with a chronic condition requires flexibility and self-compassion. Instead of focusing on grand objectives, break your aspirations into smaller, achievable steps. For example, rather than aiming to “never miss work,” set a goal to develop better communication with your employer about accommodations. Regularly review and adjust your goals based on your current health status, celebrating progress while acknowledging that setbacks are part of the journey.
Maintaining Perspective
Your condition influences your life but doesn’t define it. Practice noticing aspects of your identity beyond endometriosis – your relationships, interests, achievements, and values. Keep a record of good days and successful strategies, creating a personal reference for times when symptoms feel overwhelming. Remember that managing a chronic condition is a skill that develops over time, with each experience providing valuable information about what works for you.
Self-Advocacy Skills
Knowledge is a powerful tool for building resilience. Stay informed about your condition through reliable medical sources, but avoid overwhelming yourself with worst-case scenarios. Keep detailed records of your symptoms, triggers, and successful management strategies to share with healthcare providers. Learn to communicate your needs clearly, whether with medical professionals, employers, or loved ones. Trust your experience and intuition about your body while remaining open to new management strategies.
Conclusion
Managing the psychological aspects of endometriosis is as crucial as addressing its physical symptoms. By understanding and challenging maladaptive thinking patterns, you can develop stronger coping mechanisms and improve your overall quality of life.
Remember that experiencing these thought patterns doesn’t indicate weakness – they’re common responses to managing a complex chronic condition. The key is developing awareness and gradually building more adaptive thinking patterns while maintaining self-compassion.
The strategies outlined in this article aren’t meant to replace medical treatment but to complement it. Consider them tools in your broader management toolkit. Some days will be harder than others, and that’s okay. Progress isn’t linear, but each step toward healthier thought patterns contributes to better overall wellbeing.
If you find yourself consistently struggling with these thoughts, consider reaching out to a mental health professional who specializes in chronic health conditions. They can provide personalized strategies and additional support for your specific situation.
Your experience with endometriosis is unique to you. Take what resonates from these strategies and adapt them to fit your needs. With time and practice, you can build resilience while honoring both your challenges and your strength in facing them.
