Foreword
The COVID-19 pandemic served as a catalyst for a rapid transformation in many sectors, with digital mental health emerging as a promising frontier. As the world grappled with lockdowns, social isolation, and unprecedented stress, the demand for accessible mental health support soared. Digital interventions appeared to be the ideal solution—offering scalability, convenience, and the ability to bridge gaps in traditional healthcare systems.
Four years on, the landscape of digital mental health is a paradox of immense potential yet unfulfilled promise. Despite the initial surge in adoption and the optimism shared by key opinion leaders (KOLs), digital mental health has not fully broken through the barriers to become a mainstream component of mental healthcare.
Challenges in Integration and Adoption
One of the primary hurdles has been the lack of substantial budgets allocated to digital mental health initiatives. While there is acknowledgment of their importance, funding has not matched the enthusiasm. This financial hesitancy stems from uncertainties about the return on investment, the effectiveness of digital tools compared to traditional therapies, and the best practices for their implementation.
Reimbursement models have also lagged behind. Insurance companies and public health systems often lack clear policies for covering digital mental health services. This ambiguity creates a disincentive for healthcare providers to incorporate these tools into their practice and for patients who may be unwilling or unable to pay out-of-pocket expenses.
Integration into existing healthcare systems presents another significant challenge. Electronic health records (EHRs) and clinical workflows are not uniformly equipped to incorporate data from digital mental health tools. This disconnect hampers the continuity of care and limits the potential for these tools to inform clinical decision-making.
The Gap Between Belief and Practice
The consensus among mental health professionals and KOLs is that digital interventions are a critical component of the future of mental healthcare. They offer opportunities for early intervention, personalized care, and reaching underserved populations. However, the enthusiasm at the leadership level has not fully translated into practical, system-wide changes.
Several factors contribute to this gap:
- Evidence and Validation: Skepticism persists regarding the clinical effectiveness of digital interventions. More large-scale, peer-reviewed studies are needed to convince stakeholders of their value.
- Regulatory Frameworks: The regulatory environment for digital health tools remains complex and fragmented, making it difficult for new entrants to navigate and for existing systems to adopt innovations confidently.
- User Engagement: Many digital mental health products struggle with user retention and engagement, raising questions about their long-term efficacy.
Moving Forward
To pave the way for digital mental health to reach its full potential, concerted efforts are required in several areas:
- Investment in Research and Development: Allocating funds toward rigorous research can build the evidence base needed to support the effectiveness of digital interventions.
- Policy and Reimbursement Reform: Clear guidelines and reimbursement models will encourage adoption by providers and accessibility for patients.
- System Integration: Developing interoperability standards will facilitate the seamless integration of digital tools into healthcare systems, enhancing their utility and impact.
- Focus on User-Centered Design: Prioritizing engagement and adherence through user-friendly design and personalization will improve outcomes and sustain usage.
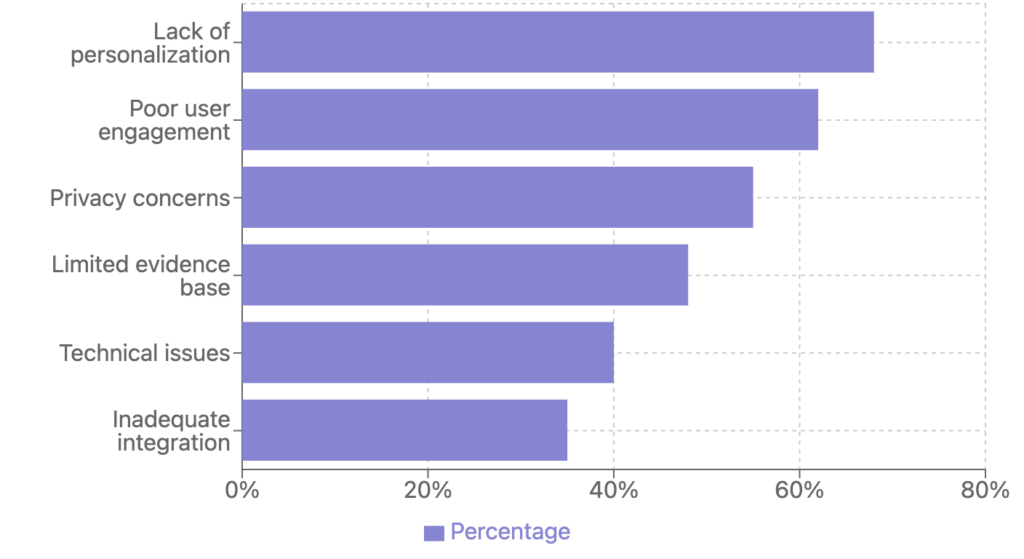
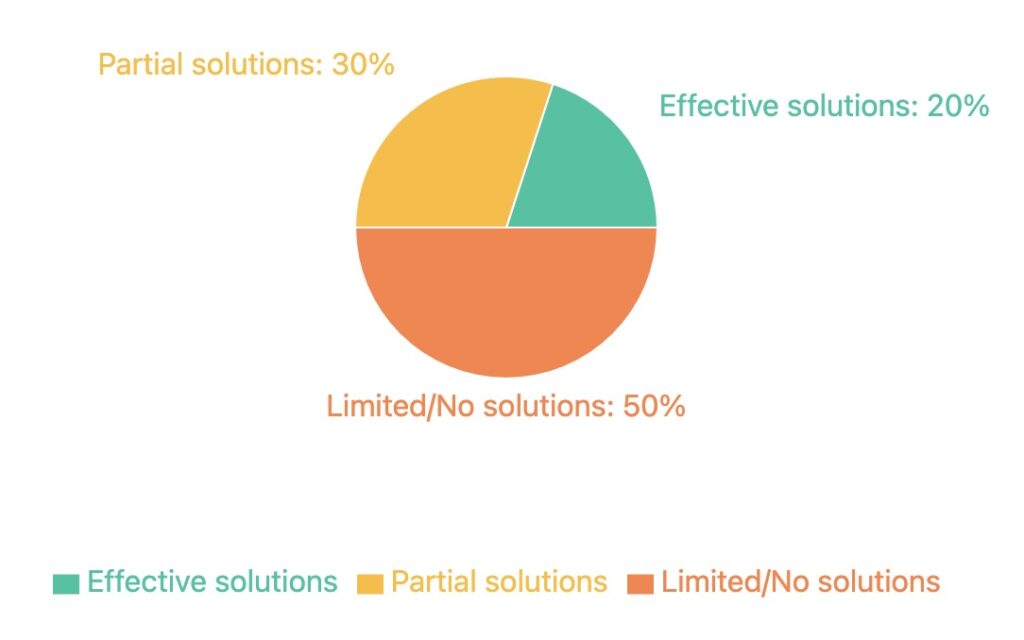
Section 1: The Digital Health Graveyard – Why Most Digital Health Products Fail
The advent of digital technology has promised a new era for mental health care, offering tools that are accessible, scalable, and potentially transformative. Yet, despite the proliferation of mental health apps and platforms, many have not lived up to their potential. This has led to a metaphorical “digital health graveyard,” filled with products that failed to make a lasting impact. Understanding the reasons behind these failures is essential for developing effective digital interventions moving forward.
Lack of Evidence-Based Foundations
A significant number of digital mental health products lack grounding in scientific research or clinical evidence. Without rigorous testing and validation, it’s unclear whether these tools are effective or safe. Users may not experience the benefits advertised, leading to disappointment and mistrust. Moreover, healthcare professionals are hesitant to recommend interventions that aren’t backed by empirical data, limiting the integration of these products into standard care practices.
User Engagement Challenges
Initial downloads and user sign-ups do not guarantee sustained engagement. Many digital health products see a steep decline in active users after the first few weeks. This drop-off is often due to a lack of personalization, monotonous content, or failure to demonstrate value over time. Without engaging features that adapt to user needs and preferences, maintaining long-term interest is challenging.
Privacy and Security Concerns
Mental health data is highly sensitive. If users perceive that their personal information is not adequately protected, they are unlikely to continue using the product. High-profile data breaches and a lack of transparent privacy policies contribute to user skepticism. Trust is paramount; without it, even the most effective tools can fail.
Regulatory Hurdles
Healthcare is one of the most regulated industries, and for good reason. Digital health products must navigate a complex web of laws and regulations that vary by country and region. Failure to comply can result in legal penalties and damage to reputation. The regulatory process can also be lengthy and expensive, posing significant barriers for startups and smaller companies.
One-Size-Fits-All Approach
Mental health conditions are diverse and manifest differently across individuals. Products that do not account for this diversity often fail to meet the needs of their users. A lack of customization can make interventions less effective and reduce user satisfaction. Tailoring interventions to individual circumstances is crucial for meaningful impact.
Section 2: Key Approaches and Their Underlying Theories
The evolution of digital technology has paved the way for innovative mental health interventions grounded in established psychological theories. These digital approaches aim to make mental health support more accessible, personalized, and engaging. Below are key approaches and the theories they are based upon.
Cognitive Behavioral Therapy (CBT) Online Platforms
Cognitive Behavioral Therapy is a well-established, evidence-based psychotherapy that focuses on identifying and challenging negative thought patterns and behaviors.
- Underlying Theory: CBT is based on the cognitive model, which suggests that psychological problems stem from maladaptive thinking patterns. By changing these thoughts, individuals can influence their emotions and behaviors positively.
- Digital Implementation: Online CBT platforms deliver structured therapy sessions through interactive modules, quizzes, and exercises. They often include features like thought diaries, cognitive restructuring tools, and behavioral experiments.
Mindfulness and Meditation Apps
Mindfulness and meditation apps aim to improve emotional well-being by teaching users to focus on the present moment.
- Underlying Theory: Rooted in mindfulness-based stress reduction (MBSR) and mindfulness-based cognitive therapy (MBCT), these practices help individuals become aware of their thoughts and feelings without judgment.
- Digital Implementation: These apps provide guided meditations, breathing exercises, and mindfulness practices. They often track progress and send reminders to encourage regular use.
Digital Therapeutics
Digital therapeutics are software-based interventions that deliver evidence-based therapeutic treatments to prevent, manage, or treat a medical disorder or disease.
- Underlying Theory: They are based on clinical research and are often subjected to regulatory approval processes similar to traditional medical devices or medications.
- Digital Implementation: These interventions are prescribed by healthcare providers and can include modules for managing chronic conditions, mental health disorders, or substance abuse.
Behavioral Activation Tools
Behavioral activation focuses on encouraging individuals to engage in activities that are aligned with their values to combat depression.
- Underlying Theory: The approach is based on the idea that increasing engagement in meaningful activities can improve mood and reduce depressive symptoms by providing positive reinforcement.
- Digital Implementation: Apps guide users to set goals, schedule activities, and track their moods to reinforce positive behaviors and break the cycle of avoidance.
Social Support Networks
Digital social support networks provide platforms for individuals to share experiences, offer mutual support, and build a sense of community.
- Underlying Theory: Social support is a critical factor in mental health, with peer interactions contributing to reduced feelings of isolation and improved coping strategies.
- Digital Implementation: Online forums, group chats, and peer support apps enable users to connect with others facing similar challenges, often moderated by professionals to ensure safety.
By integrating these evidence-based approaches into digital formats, mental health interventions become more accessible and adaptable to individual needs. Understanding the theories behind these tools enhances their credibility and effectiveness, fostering greater acceptance among users and healthcare professionals alike.
Section 3: Game-Like Interventions and How Active Self-Help Tools Can Engage Users
The integration of game-like elements into mental health interventions has emerged as an innovative approach to enhance user engagement and effectiveness. By making self-help tools more interactive and enjoyable, these interventions encourage users to take an active role in managing their mental health.
Gamification Elements in Mental Health Tools
- Points, Badges, and Leaderboards: Implementing a reward system motivates users to complete tasks and reach goals.
- Example: Earning points for logging moods or completing therapy exercises, which can unlock badges or move the user up on a leaderboard.
- Progress Tracking: Visual representations of progress, such as progress bars or level-ups, provide immediate feedback and a sense of accomplishment.
- Example: A progress bar that fills up as the user completes daily meditation sessions, encouraging consistency.
- Challenges and Quests: Setting tasks as challenges or quests adds a sense of adventure and purpose.
- Example: A 7-day anxiety reduction challenge that guides users through daily coping strategies.
Interactive Storytelling and Role-Playing
- Narrative Experiences: Engaging stories that users can relate to help in understanding and processing their own experiences.
- Example: A game where the user helps a character navigate social situations, indirectly teaching social skills and anxiety management.
- Role-Playing Scenarios: Allowing users to assume roles can help them practice responses to real-life situations in a safe environment.
- Example: Simulations where users practice assertiveness or conflict resolution.
Biofeedback and Real-Time Adaptation
- Physiological Feedback Integration: Using data like heart rate or breathing patterns to inform the intervention.
- Example: A game that adjusts difficulty based on the user’s stress levels measured through a wearable device.
- Adaptive Content: Personalizing the experience based on user input and progress to keep the content relevant and challenging.
- Example: Increasing the complexity of relaxation exercises as the user’s proficiency improves.
Social Interaction and Support
- Community Features: Incorporating social elements such as team challenges or sharing achievements fosters a sense of belonging.
- Example: Users collaborating to achieve a common goal, like a collective mindfulness milestone.
- Peer Support: Facilitating connections between users for mutual encouragement and accountability.
- Example: Chat functions or forums where users can discuss progress and offer support.
Underlying Theories and Benefits
- Self-Determination Theory: Suggests that fulfilling needs for autonomy, competence, and relatedness enhances motivation.
- Application: Games that allow users to make choices, develop skills, and connect with others can increase intrinsic motivation.
- Behavioral Activation: Engaging in meaningful activities can combat depression by increasing positive reinforcement.
- Application: Game tasks that encourage users to participate in real-life activities they enjoy.
- Cognitive Behavioral Principles: Challenging negative thought patterns through interactive exercises.
- Application: Games that present scenarios requiring the user to identify and reframe cognitive distortions.
Evidence of Effectiveness
- Increased Engagement: Gamified interventions often see higher user retention and completion rates compared to traditional methods.
- Example: Studies showing that users are more likely to complete a full course of therapy exercises when presented in a game format.
- Improved Outcomes: Research indicates that game-like interventions can lead to significant reductions in symptoms of anxiety and depression.
- Example: Clinical trials where participants using a gamified app reported better mood and coping skills.
Challenges and Considerations
- Balance Between Fun and Therapy: Ensuring that the game elements do not overshadow the therapeutic content.
- Solution: Designing games where fun and therapy are seamlessly integrated.
- Accessibility and Inclusivity: Making sure the interventions are accessible to users of different ages, cultures, and abilities.
- Solution: Offering customizable settings and content that cater to diverse user needs.
- Data Privacy: Protecting sensitive user data collected through the app.
- Solution: Implementing robust security measures and transparent privacy policies.
By incorporating game-like features into self-help tools, mental health interventions become more engaging and user-friendly. These active approaches empower individuals to participate in their mental health journey actively, potentially leading to better adherence and improved outcomes.
Section 4: Family and Caregiver Support – How Involving Family Members Can Help
The role of family and caregivers in mental health interventions is increasingly recognized as a critical component of effective treatment. Involving these support systems can enhance engagement, improve outcomes, and provide a more holistic approach to mental health care. Digital interventions are uniquely positioned to facilitate this involvement through accessible platforms and tools designed to include family members in the therapeutic process.
The Importance of Family and Caregiver Involvement
- Enhanced Support Network: Family members can offer emotional support, encouragement, and practical assistance, which can be vital for individuals managing mental health conditions.
- Improved Treatment Adherence: Involvement of caregivers can lead to better adherence to treatment plans, as they can help monitor progress and remind individuals of therapeutic activities.
- Early Detection of Symptoms: Family members are often the first to notice changes in behavior or mood, enabling earlier intervention and support.
- Reduction of Stigma: Open communication within families about mental health can reduce stigma and foster a supportive environment for recovery.
Digital Tools Facilitating Family and Caregiver Support
Collaborative Care Platforms
- Shared Access to Treatment Plans: Digital platforms can allow individuals to share aspects of their treatment plans with family members, fostering transparency and collaboration.
- Example: Apps that let users grant access to certain modules or progress trackers to trusted family members.
- Joint Goal Setting: Tools that enable families to set and work towards common goals can strengthen relationships and provide mutual support.
Communication and Messaging Apps
- Secure Messaging: Encrypted communication channels allow for private discussions between individuals, family members, and healthcare providers.
- Example: Apps that offer secure messaging for scheduling, check-ins, and sharing updates.
- Video Conferencing Features: Virtual meetings can include family members in therapy sessions when appropriate, facilitating family therapy and group support.
Educational Resources for Caregivers
- Information Libraries: Providing access to articles, videos, and courses about mental health conditions helps caregivers understand what their loved ones are experiencing.
- Example: Platforms that offer caregiver-specific content on managing symptoms, communication strategies, and self-care.
- Skill-Building Modules: Interactive modules can teach caregivers how to respond to crises, support treatment adherence, and create a supportive home environment.
Progress Monitoring and Feedback
- Shared Tracking Tools: With consent, caregivers can monitor symptoms, medication adherence, and mood logs, allowing for timely support when needed.
- Example: Mood tracking apps that send alerts to caregivers if significant changes are detected.
- Feedback Mechanisms: Caregivers can provide input on observed behaviors or triggers, contributing to a more comprehensive understanding of the individual’s condition.
Support Communities for Caregivers
- Peer Support Groups: Online forums and groups where caregivers can connect, share experiences, and offer mutual support.
- Example: Social platforms dedicated to caregivers of individuals with specific mental health conditions.
- Professional Guidance: Access to mental health professionals who can offer advice and answer questions in group settings.
Benefits of Involving Family and Caregivers
- Holistic Approach to Treatment: Incorporating family dynamics into treatment can address environmental factors influencing mental health.
- Empowerment of Caregivers: Educated and supported caregivers are better equipped to assist their loved ones effectively.
- Improved Outcomes: Studies have shown that involving family members can lead to reduced symptoms, lower relapse rates, and enhanced overall well-being.
- Strengthened Relationships: Collaborative efforts can improve communication and understanding within the family, strengthening relationships.
Challenges and Considerations
- Privacy and Consent: It’s essential to respect the individual’s autonomy and confidentiality. Digital tools must ensure that data sharing occurs only with informed consent.
- Solution: Implementing strict privacy settings and consent forms within apps to control what information is shared and with whom.
- Family Dynamics: Not all family relationships are supportive. Care should be taken to assess the suitability of involving certain family members.
- Solution: Offering options for individuals to select trusted supporters or to opt-out of family involvement features.
- Digital Literacy: Variations in comfort and ability to use technology among family members can limit the effectiveness of digital interventions.
- Solution: Providing user-friendly interfaces and tutorials to assist less tech-savvy users.
- Cultural Sensitivity: Cultural differences can influence perceptions of mental health and family involvement.
- Solution: Customizing content and approaches to be culturally appropriate and relevant.
Case Examples
- Schizophrenia Management: Apps that include family members in monitoring symptoms and medication can help manage conditions with psychotic features.
- Youth Mental Health: Platforms that engage parents in therapy exercises for children and adolescents can enhance the effectiveness of interventions.
- Chronic Illness Support: For conditions like bipolar disorder, caregiver involvement in tracking mood cycles can assist in early intervention.
Future Directions
- AI and Personalization: Leveraging artificial intelligence to personalize the caregiver’s role based on the individual’s needs and family dynamics.
- Integration with Healthcare Systems: Seamless integration of digital tools with electronic health records to keep all parties informed and involved.
- Global Accessibility: Expanding access to underserved populations by offering multilingual support and low-bandwidth options.
By embracing the role of family and caregivers, digital mental health interventions can provide a more comprehensive support system. Involving loved ones not only aids the individual in their recovery journey but also empowers families to contribute positively, fostering environments that promote long-term mental well-being.
Section 5: Conclusions
The landscape of mental health care is undergoing a significant transformation, propelled by advancements in digital technology. The potential for digital interventions to make mental health support more accessible and effective is immense. However, realizing this potential requires careful consideration of several critical factors highlighted throughout this discussion.
The Importance of Evidence-Based Design
Digital mental health tools must be grounded in robust scientific research and clinical evidence. Without this foundation, interventions risk being ineffective or, worse, causing harm. Evidence-based design ensures that the tools not only deliver on their promises but also gain the trust of users and healthcare professionals. It is essential for developers to collaborate with mental health experts and incorporate validated therapeutic approaches into their products.
User-Centered Development
Engagement is a cornerstone of effective digital interventions. By prioritizing the needs, preferences, and feedback of users, developers can create tools that are both appealing and effective. Personalization, adaptability, and interactive features can significantly enhance user experience. Employing strategies like gamification and interactive storytelling, as discussed, can sustain user interest and encourage active participation in their mental health journey.
The Role of Support Systems
Involving family members and caregivers amplifies the impact of digital mental health interventions. Support systems provide additional layers of encouragement, accountability, and understanding. Digital platforms that facilitate this involvement can lead to better adherence to treatment plans and improved outcomes. Respecting privacy and ensuring informed consent are paramount when integrating these features.
Future Directions in Digital Mental Health
The future of digital mental health interventions is promising, with emerging technologies poised to address current limitations and expand capabilities:
- Artificial Intelligence (AI): AI can personalize interventions by analyzing user data to tailor content and recommendations. Chatbots and virtual therapists can provide immediate support and triage users to appropriate resources.
- Virtual Reality (VR) and Augmented Reality (AR): VR and AR offer immersive experiences that can be used for exposure therapy, relaxation techniques, and skills training in controlled environments.
- Wearable Technology: Integration with wearable devices allows for real-time monitoring of physiological indicators, enabling timely interventions and more accurate tracking of progress.
- Big Data and Analytics: Leveraging large datasets can enhance our understanding of mental health trends, leading to more effective population-level interventions and policy-making.
Call to Action
The successful development and implementation of digital mental health interventions require collaboration among various stakeholders:
- Developers and Technologists: Innovate with a focus on evidence-based practices and user engagement.
- Mental Health Professionals: Provide expertise to ensure interventions are clinically sound and meet the needs of users.
- Researchers: Conduct rigorous studies to validate the effectiveness of digital tools and contribute to the growing body of evidence.
- Policy Makers and Regulators: Create frameworks that promote innovation while ensuring safety, privacy, and efficacy.
- Users and Advocates: Participate in the development process by providing feedback and advocating for tools that address real needs.
Final Thoughts
Digital interventions have the potential to revolutionize mental health care by making it more accessible, personalized, and effective. By learning from past failures and building on proven strategies, stakeholders can create sustainable solutions that address the diverse needs of individuals worldwide. The journey towards better mental health is a collective effort, and embracing technology thoughtfully can lead to meaningful progress in overcoming the challenges faced in mental health care today.